Resus
Being a doctor means you're no stranger to resuscitation. In the NICU, the protocol gets activated every day. Premature babies pick up infections like a sponge and within hours can decompensate. This is an unusual story of resuscitation that shouldn't have happened.
It was a typical call in the NICU, hearts racing and anxiety on 80% baseline. Being the only senior on call, I had to supervise the more junior doctor with me while we hold down admissions from the Operating Theatre, Births Department, Antenatal ward, and of course.. any Goddamn thing that came through the door.
It was 6:35 am, about an hour and 30 minutes to go before I clock out, and the phone rings. "Flat baby in Births, room 2, we need a pediatrician NOW!"
Being the only doctor available, I dropped the phone back on the charging station and grabbed my emergency box and stethoscope. Post covid, my SPO2 only just recently returned to above 90%, so the short run from NICU to Births Department had me winded.
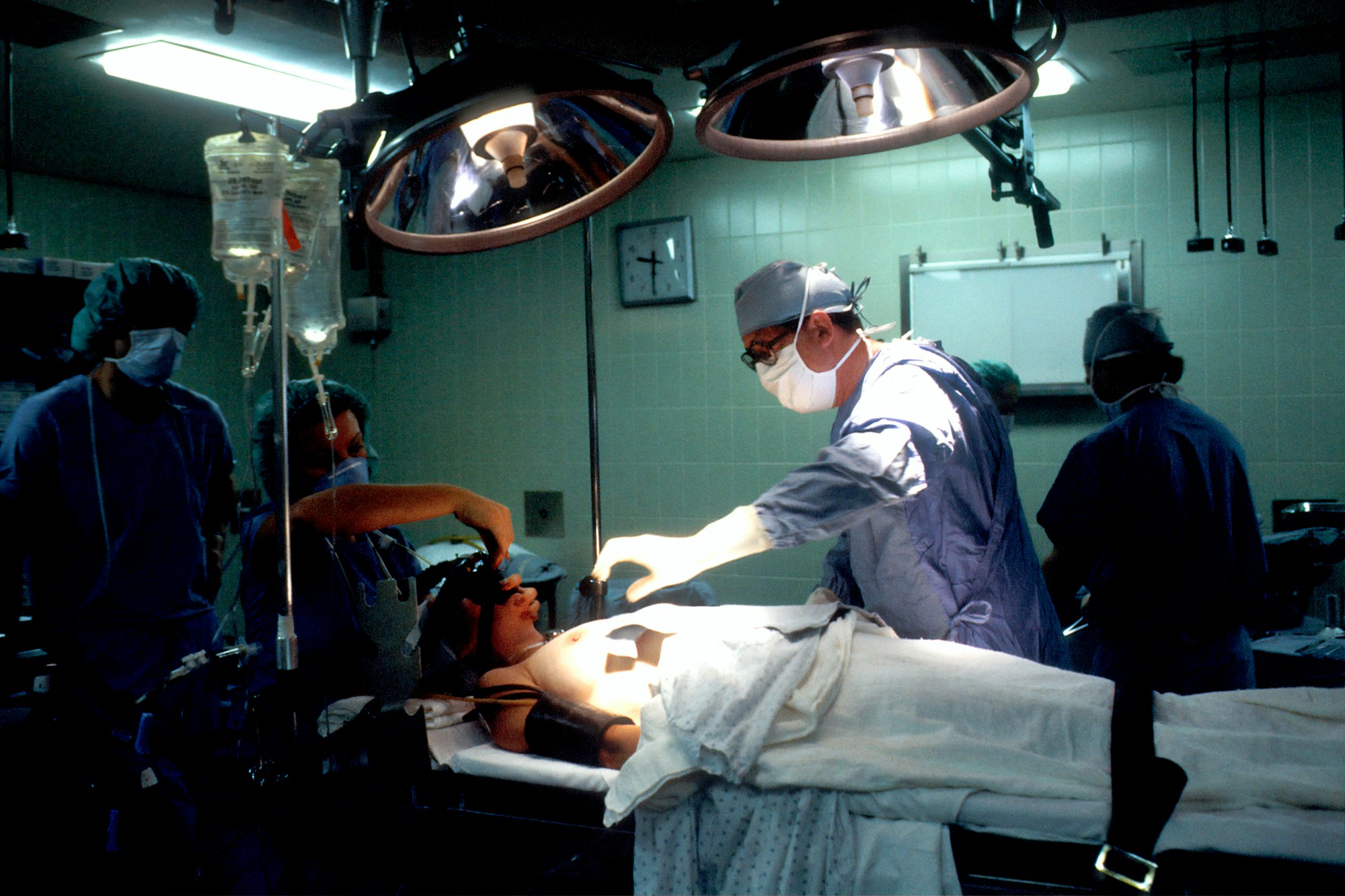
I got into room 2 and the first thing that greeted me was the nurses already starting NRP and doing chest compressions and giving emergency breaths with the AMBU bag. This was new. In all the deliveries I've supervised in my 3 years in this hospital, I've never seen chest compressions already started. The protocol only mandates compressions after rescue breaths and PPV for at least 30 seconds and of course, ideally after intubating. I asked the nurse why were compressions started. "Baby came from the ambulance.", a nurse responded. "Born before arrival.", said another.
That made some sense, so I took over the resuscitation. It was about 1 minute since arriving and since compressions and rescue breaths were given, it was time for the next step. I didn't waste time intubating the patient. Securing an Endotracheal airway, I called for my second pediatrician. The next part of resuscitation is to establish venous access. Usually, this is done through the umbilicus. The patient pampers were covering the stump so I exposed the patient...and stared. By this time, my assistant doctor arrived and I could hear the ongoing "One and two and three and breathe, one and two.." of the resuscitation continuing. There was no stump! It had completely healed over. This small and frail baby was in fact an infant!
I allowed the initial shock to pass and within a second or two I was back at the head of the resuscitation. I tried in vain to get an IV access knowing now that I was limited to that, endotracheal or intraosseous. This baby came to the hospital without a heartbeat, nor any signs of life, and was probably dead for hours. Yet, the law mandates a full resuscitation. After all, at that moment, I could be wrong, Perhaps the child had only just arrested. At the 2-minute mark, no surprise that there wasn't a heart beat. I pushed the adrenaline down the endotracheal tube.. The cycle restarted.
Now was the tricky bit. Being a specialist neonatal and obstetric hospital, we are not equipped to deal with general patients. I called the mother in to verify the child's age. "Three weeks", she replied. Fuck.
Legally that puts me squarely in the grey area of 'do I continue this resus here' or 'should I carry the baby to PED next door to the other hospital'. "4 minutes!" my assistant said, prompting the time for the second reassessment of the resuscitation. No heartbeat. I called my senior and quickly explained. She said she was going to call the consultant and hung up. "One and two and three and breathe", the chanting continued.
About 2 minutes later the phone rang. My senior called saying she contacted the other hospital and the consultant. Permission was given to continue the resuscitation here. Whew!
Now without the legal semantics out of the way, I could focus on the one thing I really supposed to do, resuscitate. I joined in on the "One and two and three and breathe."
This wasn't an experience I was keen on writing about, but my wife did say I should write about my experiences more. Admittedly she thinks I usually have all the weird cases at work. The take-home point here is that everyone involved learned something: the ambulance staff shouldn't assume every baby should be brought to our hospital, the senior doctors now know that they can continue a resus when a baby is brought to the wrong hospital (albeit with permission), and that exhausted mothers can harm their baby unintentionally (I left out the details of this case intentionally). The post-mortem was followed up by PED and Children's Authority and the Police both have active investigations ongoing as to the cause of death. For me, I learned that when the shit hits the fan, I don't sink, I swim.
