The Silent Chest
Coping with the many emotions unfolding within the physician as their patient moves through all the stages of shock and ultimately their death.
There's a saying in medicine that for a doctor, his final exam awaits him in his practice. Not an exam that includes passing the boards or renewal of some previously earned degree; but a so-called exam based on dealing or coping with the sickness and death of our patients. Some doctors, do not pass this exam and to some of them, it is overwhelming.
On witnessing the passing of a patient, many emotions emerge, unfolding from within the physician as the patient moves through each stage of shock. Confusion, blended with panic and fear takes root, and all eyes stay fixed on the doctor for leadership.
I vividly remember in my internship years, being called to a cardiology ward to review a 44-year-old patient with chest pain. Simple enough. When I arrived, the patient was sitting up in bed, actively huffing and puffing the oxygen from a facemask he wore. He was sweating and irritable at rest, both ominous signs for a cardiology patient.
As I began to ask the basic questions to assess his status, he started decompensating. His irritableness became overt deliria. The 200-pound man then began tearing off his facemask, screaming he is about to die. He screamed to call his family, he wants to tell them he was dying. The nurses and I struggled to pacify the man, and we urgently called for help. When the seniors arrived, he crashed abruptly. His exhausted heart had suddenly stopped. The ACLS protocol was immediately started and chest compressions began. I was the one pushing his ribs down against his spine to compress his heart, effectively "pumping" it. This circulates about 30% of preload to the rest of the patient's body, though not nearly as enough as a heart normally does on its own, it's at least something. Sadly, in this case, this 30% something wasn't enough, and after multiple rounds of adrenaline, the patient succumbed and his family was notified. Being the first case of a young patient having a massive and fatal infarction before my eyes, it really did leave me shook. After compressions, I walked over to the supply room, where I hoped was out of earshot of the others, and vomited into the sink. I don't know if it was because of the repeated rounds of chest compressions I had just done, but I believe a part of me knows that this was the first encounter with mortality and perhaps this visceral response reflected the inadequacies of my medical training in confronting it.
These moments came back to me about a month ago when reviewing a young 8-year-old male on my ward who recently suffered an asthmatic attack. He was treated for his initial attack in casualty and came up to my ward for conversion to an MDI and eventual discharge. It was all going according to plan, however, in the morning during our daily rounds, it was noticed he was in mild-to-moderate respiratory distress while on the inhaler. Not alarming at the time, but definitely foreshadowing what was to come. He was reviewed by a colleague in the afternoon and found to still be in this state of distress and a stat salbutamol nebulization was ordered. He was then placed for another review after this to which I remained on the ward to see done.
Walking into the room, I noticed something was not right. He was in obvious discomfort, speaking loudly. Louder than what is socially acceptable. I asked the grandmother what is wrong. She shrugged and said she doesn't know what happened to him as he was clinically fine a few minutes earlier. He then ran to the bathroom screaming incoherently. I followed, still confused, as he ripped off his pants and sat on the toilet, then started screaming for water. His grandmother brought it immediately and he tried to drink it but immediately spat it out and screamed he couldn't breathe. I then suddenly knew what was happening. He was right over the edge of the cliff of acute bronchospasm, and about to fall into the precipice of the silent chest. This is where the air channels of the lungs are so closed off by inflammation and secretions that there is little to no air reaching the alveoli; the distal place in the lung where gas exchange occurs. It is confirmed by listening to the chest with our stethoscope and not hearing breath sounds. A silent chest is a medical emergency, the patient has minutes, and in a pediatric case where their functional reserve is far less than an adult's, perhaps seconds. I grabbed him, placed him on the bed, and held him there while help was called.
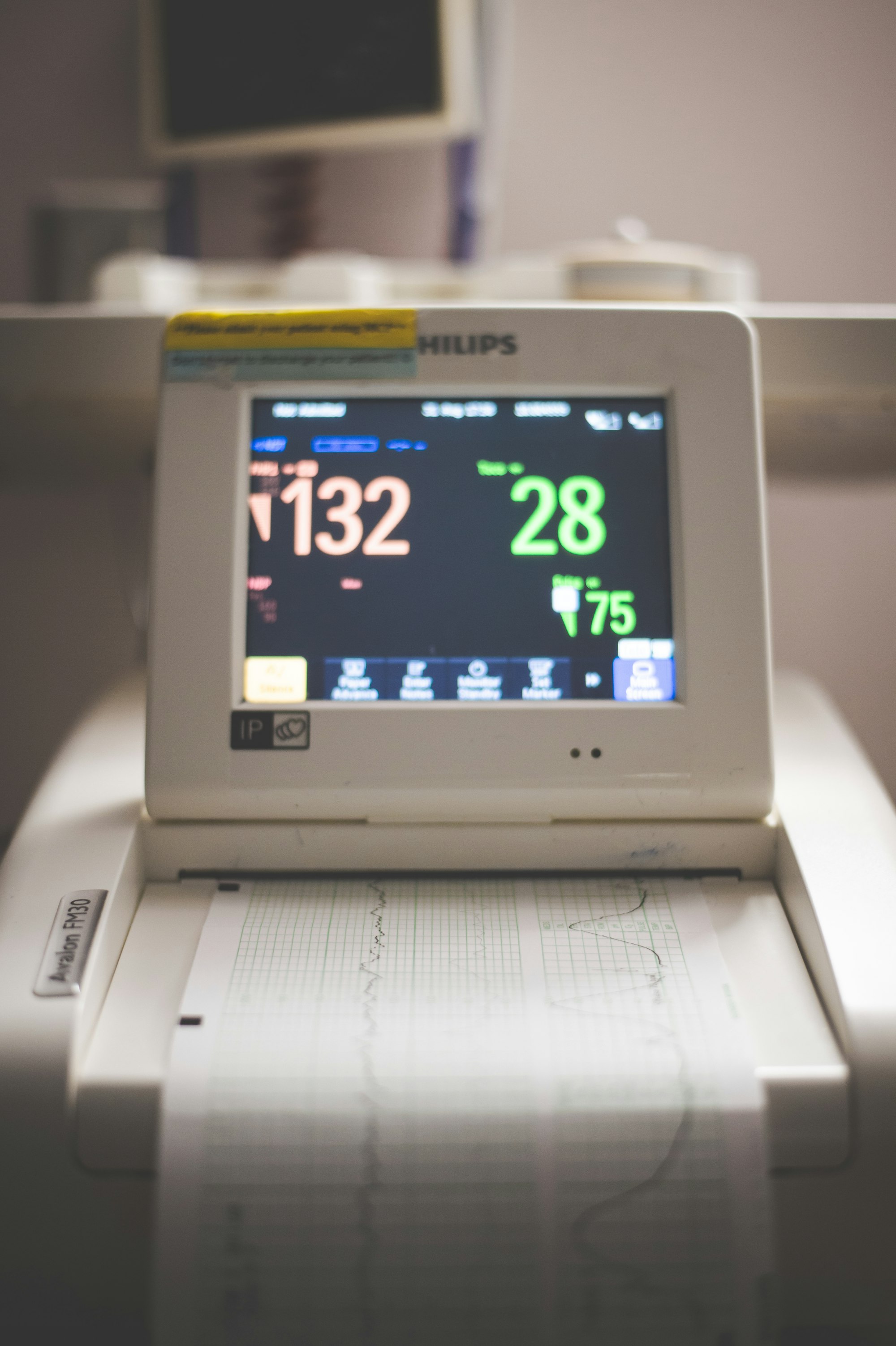
His screaming continued and then became combative, attempting to rip off his oxygen mask that was immediately placed, and kick the hospital staff who continued to hold him. A vitals machine was obtained, and his SPO2 levels were measured as best as we could... 38%. Knowing that an SPO2 machine obtains its values from infrared absorption of blood measured by the manufacturer in patients with known blood oxygen levels, an SPO2 of less than 80% is unreliable since blood samples for this population sparsely exist as they would need emergency treatment rather than academic blood sampling. Therefore a dismal SPO2 reading of 38% was obtained by graphical extrapolation and very likely, an overestimation.
More doctors then arrived, Salbutamol and Atrovent nebs were given continuously and large bore IV accesses were obtained. A crystalloid bolus was given to optimize preload and a magnesium infusion started. At this point, his SPO2 levels were nearing 99% but he had no response to pain. His GCS score was effectively 3/15. The lowest that can be given and equal to someone already deceased. The Pediatric ICU was called and responded immediately. The patient's care was then handed over to the intensivists.
These moments exist uniquely for doctors, and in no other profession where it is routine to instruct teams of staff to resuscitate patients on the verge of death and then expected to carry on the rest of their daily ward tasks. To me, this should not be an accepted convention. In battle, the soldiers who return from war are screened and treated for suspected or diagnosed PTSD. Yet for doctors, we are seen as persons (or rather machines) who tolerate traumatic, and for lack of a better term, quite horrible experiences who are then told to continue working thereafter. Guidelines recommend debriefing for every death, but in practice when you have 20+ patients per ward, new admissions arriving hourly, and angry relatives and parents who seem to take pleasure in humiliating hospital staff, a debrief session seems like an ethereal luxury. The medical culture even supports this tradition by reprimanding on the physician who struggles to cope with confronting mortality. Or indirectly, by placing expectations that work should be completed without addressing properly, the 'elephant in the room'.
The patient eventually made a full recovery. His GCS score improved within minutes of his magnesium infusion, he was soon responding to pain and by morning was back to baseline with no obvious neurological deficit. Yet, for us physicians, even if patient recovers, moments of terror like these do not cease.
As recent as last week, while on-call in the Neonatal ICU, I arrived at my shift to a ventilated baby who was not improving in respiratory status. Despite starting CPAP via nasal props, his grunting and tachypnea worsened. A chest x-ray was ordered and an anterolateral pneumothorax with mediastinal shift to the contralateral side was seen. It was not large enough to cause cardiac compromise but due to his clinical state, could not be left to be reabsorbed. I had to perform an emergency chest tube on a newborn baby. To add insult to injury, the births department suddenly called during the chest tube placement and said that a preterm baby was just born with no heart rate and needed an emergency pediatrician. I won't go into the details but a central line was placed on the resuscitaire in full view of the mother and obstetric staff, the patient was intubated and chest compressions commenced. The baby received 2 rounds of adrenaline before her little heart started beating on its own.
Leaving that shift again left my mind full of these run-ins with near-patient-death and reminds me of the absolute brevity of our lives. The baby, thankfully, is now being gradually weaned off the ventilator and expected to make a full recovery from the event, though it may be too soon to tell if there would be any long-term developmental delays from birth asphyxia. As of now, we on the team are hoping there isn't.
- Gib
